Abstract
Background and Aims:
The CHA₂DS₂-VASc score is a well-established tool that predicts the risk of cerebrovascular accident (CVA) in patients with atrial fibrillation. It has also been validated to predict long-term stroke outcomes and cardiovascular disease burden in patients with and without atrial fibrillation as it encompasses most risk factors for ischemic stroke. However, it does not incorporate two important risk factors for ischemic stroke which are dyslipidemia and tobacco use. It has been well established in several studies that these risk factors confer an increased risk for stroke. We combined these risk factors with the traditional CHA₂DS₂-VASc scoring to create a novel CHA₂DS₂-VASc + score. We aimed to assess the ability of CHA₂DS₂-VASc+ scoring to screen ischemic CVA in patients without atrial fibrillation.
Methods:
This retrospective cohort study was approved by the institutional review board (IRB). The study included patients with CVA symptoms who had magnetic resonance imaging (MRI) of the brain and excluded those with atrial fibrillation, intracranial hemorrhage, history of migraine, seizure disorder, and brain tumors. We collected data on demographics, clinical presentation (facial droop, side of weakness, presence of aphasia), home medications, laboratory tests, and imaging results. For calculating the CHA₂DS₂-VASc+ score, we used the traditional parameters of the original score; congestive heart failure (CHF), hypertension, age, diabetes mellitus (DM), prior CVA or thromboembolism, hypertension (HTN), vascular disease, and sex. In addition to this, we assigned one point each, for dyslipidemia and tobacco use. The dyslipidemia criterion was a total cholesterol >240 mg/dl, triglycerides >200 mg/dl, LDL >160 mg/dl, or HDL <40 mg/dl. The criteria for tobacco use was that of a current or former smoker with more than ≥ 15 pack years history. Mann-Whitney U test was used for continuous variables and the chi-square test was used for categorical variables.
Results:
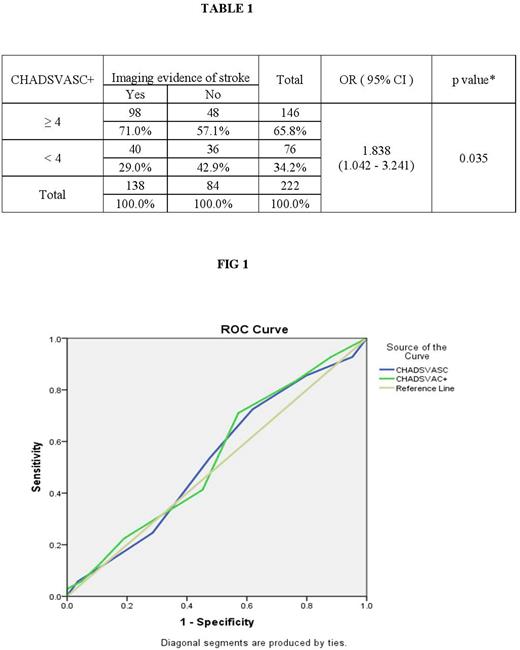
Of the total 500 patients screened, 222 patients met the inclusion criteria. There were 138 patients with MRI evidence of infarct vs 84 without evidence of infarct. Demographic data including age and sex were distributed equally between the two groups. There was no significant difference in the risk factors between the two groups which included HTN, CHF, and DM, NIHSS score, HLD, tobacco use, prior statins, antiplatelet and anticoagulant use. The CHADVASc score was equally distributed between the two groups as well. A total of 146 patients were found to have a CHA₂DS₂-VASc+ score of ≥ 4 and when this was used as a cut-off, there was a statistically significant difference seen as 71% of patients with imaging evidence of a stroke had a score of ≥ 4 vs 57.1% of patients without imaging evidence of stroke [ OR=1.838, (95 % CI: 1.042-3.241), p- 0.035] (as shown in table 1). We also calculated the CHA₂DS₂-VASc score and among patients with a score ≥ 4, only 53.6% had imaging evidence of infarct vs. 47.6% in the other group (p-0.385). The ROC curve analysis for the CHA₂DS₂-VASc+ score showed an Area of 0.539 (as in Fig 1), sensitivity of 70.3%, and specificity of 42.8%. The positive predictive value (PPV) was 66.7%, and the negative predictive value (NPV) was 46.9%.
Conclusion:
Our results indicate that CHA₂DS₂-VASc+ scoring may be a useful predictor in estimating the risk of ischemic CVA in non-atrial fibrillation patients. Smoking and dyslipidemia are well studied risk factors for CVA and including these factors in addition to the original CHA₂DS₂-VASc scoring may help increase its sensitivity. Considering the findings of our single-center study, we would recommend a large-scale prospective trial to validate the CHA₂DS₂-VASc+ score. Further studies with head-to-head comparison of CHA₂DS₂-VASc+ and CHA₂DS₂-VASc in assessing their sensitivity for predicting ischemic CVA could potentially enhance our existing tools.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal